At 6:47 AM on a Tuesday morning in the ICU, a critical care nurse reaches for her mobile device to scan a patient's medication barcode. A screen notification pops up, showing a low-battery warning. She has seven more hours left in her shift. Unfortunately, this and very similar scenarios play out in hospitals across the country every day, underscoring why battery life isn't just a technical specification but a patient safety issue.
The 12-Hour Reality of Clinical Work
Healthcare professionals, particularly nurses, frequently work 12-hour shifts or longer. This extended shift model, while controversial in some circles, has become standard across many healthcare facilities. The demands placed on mobile devices during these patient-care marathons are extraordinary: constant barcode scanning for medication verification, EHR documentation updates, secure messaging with physicians, clinical photography, vital sign monitoring, and real-time access to patient records.
The problem? Most consumer-grade mobile devices were never designed for this use case. The average battery rarely lasts that long when used constantly at the intensity required for healthcare workflows.
When Batteries Die, Workflows Break
The consequences of dead devices during clinical shifts extend far beyond inconvenience. Clinical workflows break down when the digital tools that healthcare workers rely on become unavailable. Consider what happens when a device fails mid-shift:
Medication Administration Delays: Nurses scanning patient wristbands and medication barcodes represent critical safety checkpoints. When a device dies, nurses face a choice: delay medication administration while finding a charged device or skip the electronic verification step, which is problematic from both patient safety and regulatory compliance perspectives.
Documentation Gaps: EHR systems are designed for real-time documentation. When mobile devices fail, clinicians either defer documentation (creating potential information gaps that could affect subsequent care decisions) or must locate fixed workstations, taking them away from the bedside and disrupting the mobile workflow benefits that justified the technology investment in the first place
Communication Breakdown: Modern clinical communications systems integrate voice calling, secure messaging, and alert notifications on a single device. A dead battery severs these communication channels precisely when rapid coordination among care team members is most critical.
Data Loss Risk: Cloud-based EHR systems typically buffer data locally before syncing it to central servers. If a device fails unexpectedly during active documentation, unsaved data may be lost entirely, forcing clinicians to recreate their work from memory, introducing inefficiency and the potential for error.
Research from the FDA's Medical Product Safety Network found that up to 50% of service calls in surveyed hospitals were related to battery issues, including failure to plug in battery-powered medical devices, inaccessible power outlets, and battery overcharging due to inconsistent charging practices.
Why Beam Mobile's Integrated Approach Matters
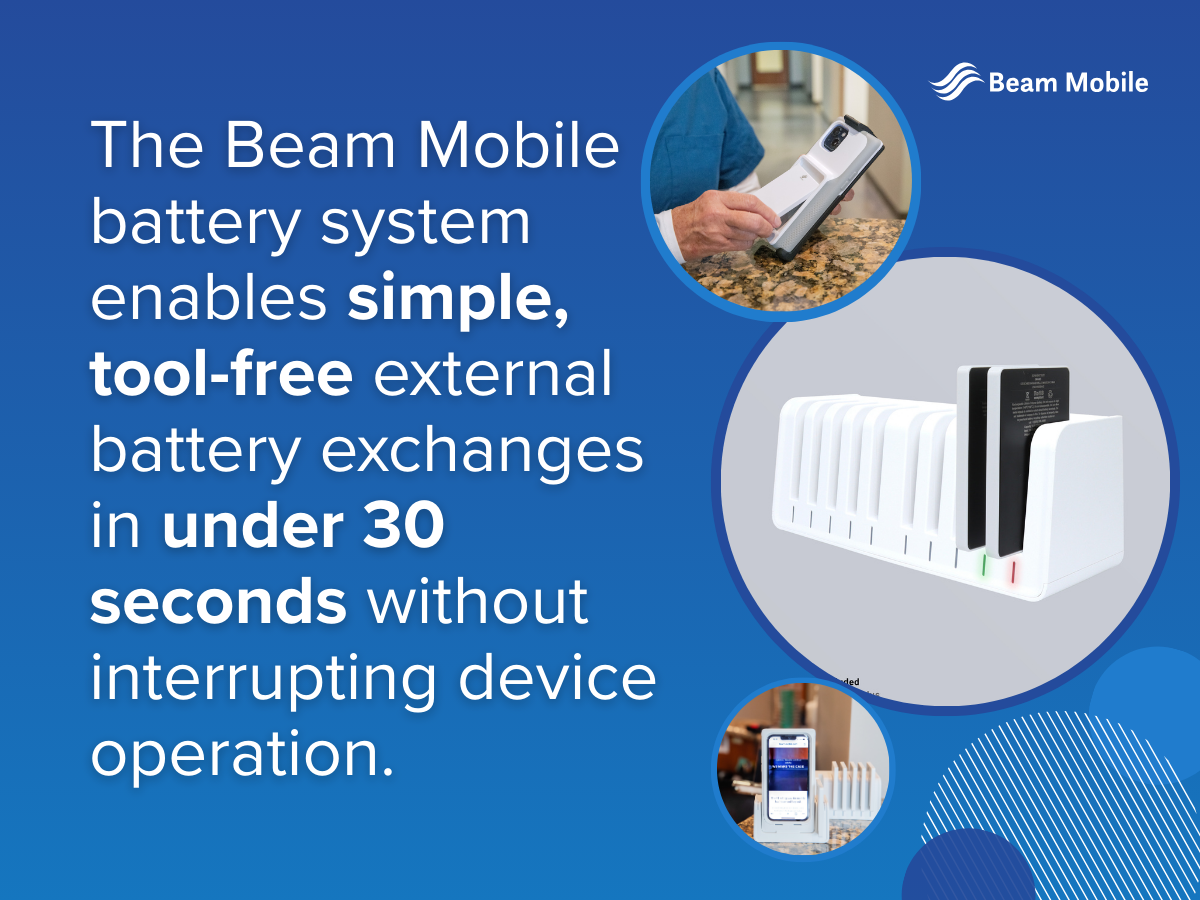
Beam Mobile has developed a comprehensive swappable battery solution tailored for healthcare mobile devices, addressing the unique challenges of 12-hour clinical shifts. The Beam Mobile swappable battery system comprises three core components:
1. Extended-Capacity Battery Packs: Beam Mobile's batteries are engineered to provide extended runtime specifically for demanding healthcare applications. Each battery pack is designed to power devices through full clinical shifts, with capacity ratings optimized for the high-intensity usage patterns of bedside care, including constant barcode scanning, EHR documentation, clinical photography, and real-time communication.
2. Rapid-Swap Design: The Beam Mobile battery system enables simple, tool-free external battery exchanges in under 30 seconds without interrupting device operation. The batteries feature ergonomic grip surfaces and clear alignment guides, allowing clinical staff wearing gloves to perform swaps quickly and confidently. The system includes audible and tactile confirmation when batteries are properly seated
3. Battery Management: Beam Mobile batteries incorporate smart charging technology with multi-stage charging profiles that optimize battery health and lifespan. The system includes:
• Visual LED indicators showing charge status
• Compatible charging stations that can charge multiple batteries simultaneously
• Temperature management to prevent overheating during rapid charging cycles
The Economics of Battery Reliability
Healthcare organizations increasingly recognize that battery-related device failures carry high hidden costs:
Staff Time: The time nurses and IT departments spend managing battery issues, searching for charged devices, and nurses traveling to fixed workstations because of battery depletion on each shift adds up quickly.
Device Replacement Costs: Devices that cannot hold a charge due to battery degradation require premature replacement.
Patient Safety Incidents: The cost of even a single adverse patient outcome attributable to device failure far exceeds the cost of implementing robust battery management systems.
Opportunity Costs: Every dollar spent on premature device replacement, additional backup devices, or powered cart infrastructure is a dollar that cannot be used for other clinical priorities.
Designing for the Reality of Clinical Workflows
The most sophisticated mobile technology infrastructure becomes worthless if devices fail during real-world use. Healthcare IT leaders are learning to evaluate mobile device solutions not by technical specifications in controlled environments but by performance in the messy reality of clinical care, and Beam’s swappable batteries are rising to the occasion.